How Graston Technique Supports Pelvic Health: A Gentle, Whole-Body Approach
When you think about pelvic floor therapy, your mind probably jumps to Kegels or internal work—but pelvic health is so much more than that. For many of my clients, especially those living with chronic pain, hypermobility, or complex conditions like Ehlers-Danlos Syndrome (hEDS), pelvic floor dysfunction isn’t just about the pelvic floor muscles—it’s about how the entire body moves, holds tension, and responds to stress.
One manual therapy technique that I often incorporate into care is Graston Technique, a gentle yet powerful tool that can help release fascial restrictions and improve soft tissue mobility in key areas influencing pelvic health.
Graston Technique Provider
What Is Graston Technique?
Graston Technique is a form of instrument-assisted soft tissue mobilization (IASTM). Using specialized stainless-steel tools, I assess and treat areas of tension or fascial “stickiness” in the body. These tools allow me to feel restrictions beneath the skin and apply gentle pressure to encourage tissue remodeling, improve blood flow, and restore mobility.
When applied with skilled, light pressure (especially important in complex or sensitive cases), these tools can:
Stimulate local circulation
Break up adhesions in the fascia
Encourage lymphatic flow
Improve neuromuscular control
Support tissue remodeling and healing
It’s commonly used in sports rehab and orthopedic settings—but when applied with clinical precision and care, it can be profoundly helpful in supporting pelvic health and whole-body function.
I’ve been Graston Technique Specialist Certified (GTS) since 2018, and over the years, I’ve developed a trauma-informed, gentle approach to using this method with complex clients—including those with hypermobility, chronic pain, and nervous system dysregulation. My goal is always to work with your body, not against it—so we can release tissue tension without triggering rebound pain or flare-ups.
Why This Matters for Pelvic Health
The pelvic floor doesn’t function in isolation—it’s part of a larger network of muscles, fascia, and nervous system pathways. Restrictions in the surrounding tissues—hips, abdominals, inner thighs, back, or even the diaphragm—can impair pelvic floor coordination, contribute to pain, and limit the success of traditional strengthening programs.
This is especially true for clients with hypermobile Ehlers-Danlos Syndrome (hEDS). In my clinical experience, the “sticky” fascia often seen in hEDS creates resistance that traps underlying muscles in dysfunctional patterns. Without addressing these restrictions first, attempts at strengthening or stabilization can backfire—leading to increased pain, tension, or fatigue. I know this firsthand because I have hEDS, and long before I was treating patients in pelvic health, I discovered Graston Technique. It was truly the first type of manual therapy that relieved the fascial pain I experience. To this day, I still use to in combination with various other forms of self-treatment to address myofascial restrictions in my body.
Because as a person with hEDS, treating my fascia NEEDS to be part of my self-care routine. By targeting the fascial layer, we create space for muscles to move freely and function more efficiently. In many cases, this is what finally allows those with severe fascial restrictions due to HSD/hEDS to access the appropriate muscles (pelvic floor, glutes, deep core muscles, etc.) that standard approaches can’t reach.
Graston can also be helpful for clients with other common comorbidities related to both hEDS and pelvic floor dysfunction:
POTS, dysautonomia, or pelvic congestion syndrome: Circulatory and lymphatic congestion can create a heavy, achy sensation in the pelvis and legs, which Graston may help alleviate by improving tissue glide and local blood flow.
Endometriosis or chronic pelvic pain: Layers of scar tissue and inflammation create fascial restrictions in the abdomen, hips, and pelvic cavity—contributing to pain and dysfunction.
MCAS: Chronic inflammation and tissue irritation can create hypersensitive fascia that benefits from slow, calming touch and improved drainage.
Not Just About Muscles—It’s About the Nervous System, Too
As an occupational therapist specializing in trauma-informed pelvic health, I always approach manual therapy with nervous system regulation in mind. That means no “scraping,” bruising, or aggressive techniques. Instead, sessions are grounded in your comfort and safety. Being Graston Certified, I learned specifically how to treat without causing bruising or skin redness (also known as petechiae.)
When the fascia begins to move more freely, the nervous system can follow suit. Many clients describe feeling lighter, more connected, and more regulated after Graston—a key piece of the puzzle when we’re working with the fight-or-flight responses that often accompany pelvic floor dysfunction and chronic illness.
Areas I Might Treat with Graston in Pelvic Health Sessions
Because fascia is a body-wide system, we may use Graston in several regions—not just the pelvis itself. Some of the areas I often treat include:
Inner thighs (adductors) – Often tight in those with chronic guarding or pelvic pain; can impact pelvic alignment and contribute to incontinence or sexual pain.
Lower abdomen – A key area for clients with C-section scars, endometriosis, digestive issues, or bladder tension.
Pubic region (external only) – Can gently address fascial tightness that affects bladder mobility and lower core activation.
Glutes and sacrum – Releases SI joint tension, supports hip mobility, and improves load transfer through the pelvis.
Obliques and rib cage – Vital for breath coordination and diaphragm-pelvic floor synergy, especially in clients with POTS or upper body tension.
TFL and IT band region – Helps reduce compensatory patterns from core instability or altered gait.
Hamstrings and calves – For those with pelvic pain linked to postural strain or peripheral tension.
Thoracic spine and back – Enhances postural alignment and supports autonomic regulation through fascial unwinding. Also allows the diaphragm to move more freely and improves backbody expansion with diagphragmatic breathing.
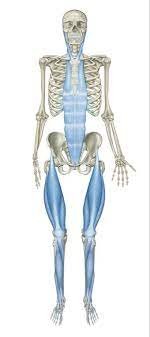
Neck and jaw – Especially helpful in cases where upper body tension is driving global nervous system dysregulation and pelvic floor guarding. Also, the fascial line from the jaw to the pelvis is a real thing!
The front fascial line connecting the jaw to the pelvis.
Every client is unique, and I always tailor the session based on your symptoms, comfort level, and health history. We may use Graston in isolation or pair it with other interventions like breathwork, neuromuscular re-education, or somatic awareness techniques.
Why My Approach Is Different
Not every provider is trained—or experienced—in using Graston for pelvic health or medically complex conditions. My approach is grounded in:
Years of clinical experience using Graston with complex clients since 2017
A trauma-informed, nervous system-based lens to ensure sessions are calming and effective—not overwhelming
Expertise in hypermobility, chronic pain, and connective tissue disorders
An occupational therapy framework, meaning I look at the whole person—not just isolated muscles or movements
You won’t find a “no pain, no gain” mentality here. Instead, we focus on safety, connection, and slow, sustainable progress.
This means you’ll get care that’s gentle, effective, and deeply respectful of your body’s story—without pushing past your limits.
Is Graston Technique Right for You?
This technique may be helpful if you’re experiencing:
Pelvic or abdominal pain
Painful sex or pelvic tension
Scar tissue from surgery, endometriosis, or birth
Urinary urgency, frequency, or leakage
Constipation or incomplete bowel emptying
Core or glute weakness that doesn’t improve with exercise
Tailbone, hip, or SI joint pain
Postpartum recovery
Tissue sensitivity or “tightness” in a hypermobile body
Symptoms related to hEDS, POTS, MCAS, or fibromyalgia
Especially if you’ve tried pelvic PT before but it didn’t help—or it made things worse—Graston may be the missing piece.
Whether you’re brand new to pelvic floor therapy or have tried other approaches that didn’t quite stick, adding gentle fascial release may be just the reset your body needs.
Want to explore if Graston could be part of your healing plan?
Let’s talk. I’d love to hear your story and help you feel safe, supported, and empowered in your body again. Click here to schedule a consultation, or send me a message with your questions. You deserve care that listens to your whole body—not just your symptoms.
This blog post is for educational and informational purposes only and is not intended as medical advice or a substitute for individualized care. Always consult with your healthcare provider before beginning any new treatment or therapy, especially if you have complex medical conditions.